
What is Sleep Apnea?
Millions of Americans suffer from sleep apnea, a sleep-related breathing disorder that causes the body to stop breathing during sleep. Sleep apnea is diagnosed by medical professionals through the use of sleep studies that measure blood oxygen level, brain activity, breathing patterns and other body functions.
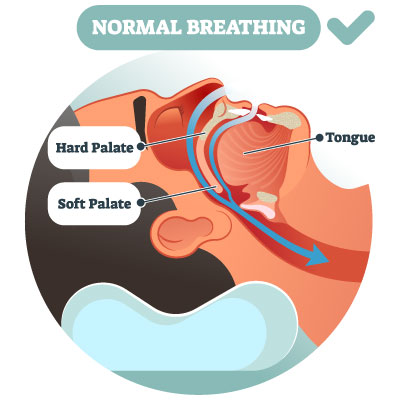
Normal Breathing
During sleep, the airway is properly supported by the throat muscles and there are no obstructions from the tongue or soft tissue. This permits the steady flow of air and oxygen to the lungs and the rest of the body.
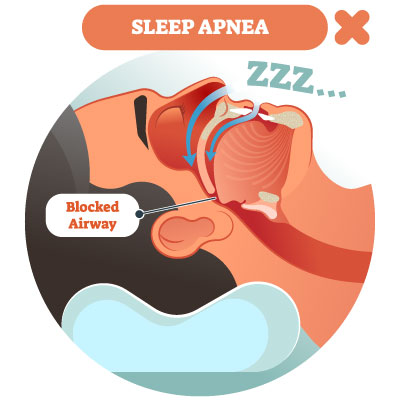
Sleep Apnea
When the tongue and soft tissue adjacent to the airway collapse and block the airway, breathing is stopped. This deprives the body of necessary oxygen and disrupts sleep as the body wakes up repeatedly to re-start breathing.
Types of Sleep Apnea
Obstructive Sleep Apnea (OSA) is the most common form of sleep apnea. During sleep, the throat muscles, tongue and mouth tissues become very relaxed. For OSA patients, these structures become loose and sag to the extent that they obstruct the airway, causing the patient to stop breathing.
Other forms of sleep apnea include Central Sleep Apnea, which occurs when the brain fails to send the signal to the body to breathe during sleep and a combination of both central sleep apnea and obstructive sleep apnea known as Complex Sleep Apnea syndrome.
Dental Sleep Medicine & Obstructive Sleep Apnea
Dentists see their patients twice a year to look for oral health problems and ask about general health issues; for most people, this is more frequently than they see their physician. Dentists that are trained in dental sleep medicine also provide screenings for obstructive sleep apnea during regular dental patient check-ups.
Macon dentist Dr. Leigh Bennett has extensive training and a practice focus on dental sleep medicine and management of TMJ disorders. She works closely with sleep physicians to provide oral appliance therapy for treatment of obstructive sleep apnea. Dr. Bennett also brings her knowledge and training to her dental patients to provide screenings for OSA in her general dentistry practice, Hartley Bridge Family Dentistry.
The OSA Apneic Event Cycle
Restful sleep is essential for healthy body function. During sleep, the body systems recharge and the brain is able to rest and refresh the communication processes within the nervous system. Learn why sleep is important.
Obstructive sleep apnea makes these and other functions of sleep nearly impossible and is considered to be a serious medical threat for the patient. For OSA patients, the body goes through repeated and harmful cycles during sleep:
- As the airway becomes partially blocked by overly relaxed muscle and soft tissue, the vibration of air moving through the narrowed opening creates the loud, rattling sound of snoring.
- When the airway becomes fully blocked, the body stops breathing involuntarily. This is known as an apneic episode or event.
- The brain registers the lack of oxygen and sends an urgent signal to the body to breathe (now!). The patient wakes up abruptly with a loud gasp or snort and begins to breathe again.
- Most OSA patients stop breathing multiple times during sleep; severe cases stop breathing as often as 30 times per hour or more. Repeatedly depriving the body of oxygen and vital rest can lead to serious (even fatal) health consequences if not treated.
Signs & Symptoms of Obstructive Sleep Apnea
Loud Snoring
Chronic, loud snoring and gasping for air are characteristic warning signs of sleep apnea. Generally the first person to complain about OSA symptoms is the patient's bed partner; the person with undiagnosed sleep apnea might not even realize that they have a problem.
While the most noticeable sign is heavy snoring and breathing cessation, other common signs and associated symptoms of obstructive sleep apnea include:
- Morning headaches
- Daytime drowsiness
- Irritability
- Insomnia
- Choking sounds during sleep
- Difficulty staying focused
- Nighttime incontinence
- Heartburn
- Depression
- Weight gain
Do You Snore? Not all snoring is related to sleep apnea. Learn more about snoring and possible causes.
Review these frequently asked questions to learn more about sleep and Obstructive Sleep Apnea:
What Causes Obstructive Sleep Apnea?
Obstructive sleep apnea affects patients of all age groups including children, however, the majority of cases reported are adult males. There are a number of health factors that are related to OSA:
- Family history of obstructive sleep apnea.
- Obesity - being overweight contributes to the accumulation of fatty tissue in the muscles near the airway. As these muscles relax, the fatty tissue can compress the airway and increase the risk of partial or full obstruction.
- Medical conditions such as congestive heart failure, lung disease, hormonal disorders, asthma and other illnesses may be linked to OSA.
- Large neck circumference - patients with a large neck often have a narrow airway, making it more difficult for air to pass through.
- Alcohol and drug use - alcohol and sedative drugs have a depressant effect on the body; they may cause the airway muscles to becoming overly relaxed and lead to an obstruction.
- Smoking causes inflammation in the upper airway and can be a contributor to obstructive sleep apnea. Nicotine from smoking is also a stimulant that disrupts sleep, which adds to the problem for OSA patients.
Medical Complications associated with Obstructive Sleep Apnea
Without treatment, sleep apnea can develop into a health crisis. When a person stops breathing repeatedly during sleep, this impacts the oxygen saturation levels in the body and increases the risk of developing heart disease, high blood pressure, stroke, diabetes and other life-threatening conditions.
Recent studies indicate that patients with sleep apnea that become infected with COVID-19 are at even greater risk of severe illness and death. Learn more about the health risks of obstructive sleep apnea.
Obstructive Sleep Apnea Diagnosis & Treatment
To confirm a diagnosis of OSA, your sleep physician or ENT (ears, nose and throat specialist) will order a sleep study to be performed at a sleep laboratory. Your sleep test will measure your respiration rate, blood oxygen level, number of apneic episodes and other vital information as you sleep. You may also be given a simplified sleep test for home use to record your breathing rate and oxygen saturation level.
Medical sleep professionals recommend treatment based on the severity of OSA. Treatment may include lifestyle changes, medication adjustments or the use of medical devices to assist with breathing and airway stability during sleep. Learn more about Treatment for Sleep Apnea.
Do you experience morning headaches and daytime drowsiness?
Check your score on our Sleep Apnea Quiz and share the results with your doctor.
It's time to enjoy restful sleep again.
Contact Hartley Bridge TMJ & Dental Sleep Center of Macon for more information about obstructive sleep apnea or a referral to a sleep physician near you.